HOW DOES BLOOD CLOT?
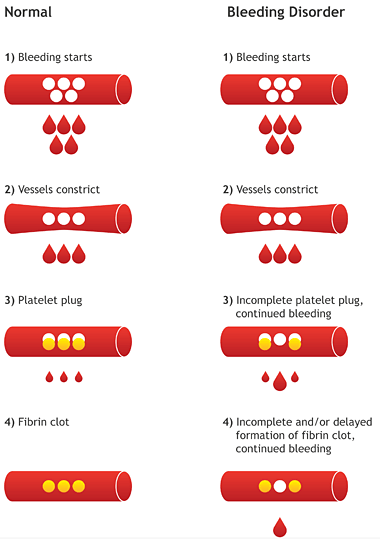
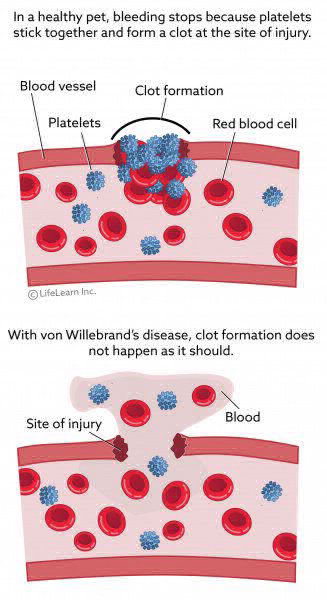
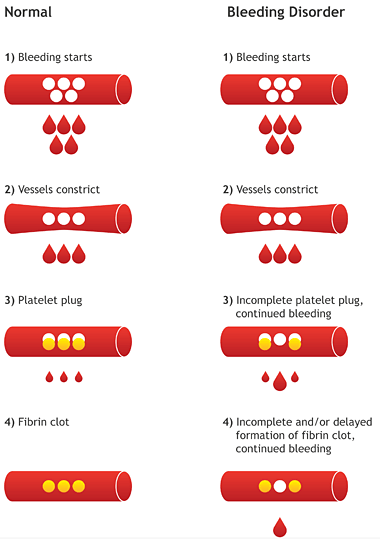
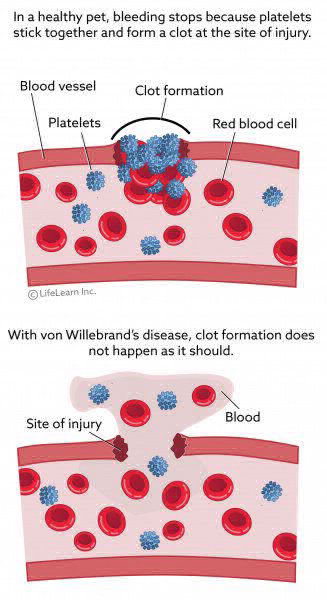
A bleed occurs when blood vessels are torn. This can happen outside the body (like a cut), or inside the body (like in a joint or muscle). The tear in the vessel causes blood to leak out into the surrounding tissues – causing a bleed.
The body reacts quickly: recruiting tiny cells called platelets, which clump together to “plug” the leak. This platelet plug attracts clotting factors to the site of the leak, which form an even stronger plug called a fibrin clot. The clot quickly stops the bleeding. This entire process is complex but happens very quickly: this is why most bleeds are quickly managed in people without hemophilia.
WHAT HAPPENS IN PEOPLE WITH HEMOPHILIA?
People with hemophilia do not produce any or enough clotting factor. So, platelets can’t clump together as well, resulting in a much weaker fibrin clot. Their blood will clot eventually, but it takes much longer than in someone with clotting factors.
HOW & WHERE BLEEDS HAPPEN
Bleeds can happen after a minor injury, such as a cut or fall. Bleeding can also happen during surgery, such as tooth extractions. In people with severe hemophilia, bleeding may be spontaneous, meaning it happens for no apparent reason. This can happen internally, or inside the body. Internal bleeds often occur within the joints (typically the knees, elbows and ankles) and muscles. The most serious bleeds are those in the vital organs. For joint or muscle bleeds, factor replacement therapy is recommended.
The most serious bleeding episodes, that can threaten a person’s life or functioning, occur in the head, neck/throat, abdomen, kidney or bladder, and the eyes. These require immediate medical attention – so visit your nearest HTC or emergency room if this happens.
TREATMENT WITH FACTOR REPLACEMENT
The most basic treatment for hemophilia is factor replacement therapy. This involves an infusion of the clotting factor a person is lacking to control bleeding. Factor replacement therapy is not the only treatment option for severe hemophilia. Your child’s doctor will determine which clotting factor they are lacking and advise if factor replacement therapy is appropriate for them; it may not be in some patients. Many patients, especially those with severe hemophilia, receive factor replacement therapy prophylactically to prevent a bleeding episode. Factor replacement is not permanent: clotting factors leave a person’s body within 2 or 3 days. So, regular treatment is required.
Every patient is different: the frequency of infusions will be a decision you make with your healthcare team. Two common approaches are:
➥ On-demand therapy. Infusions are given as soon as possible after a bleed happens to control bleeding. This is often how joint and muscle bleeds are treated. Sometimes, especially with prompt treatment, one infusion is enough. In other cases, treatment is given over several days. For more serious bleeding, a patient may need 2 to 3 infusions a day, for 10 to 14 days.
➥ Prophylaxis (preventative) therapy. Infusions are given once or more a week to help prevent bleeds. Often, children with hemophilia receive prophylaxis therapy to help prevent bleeds from happening at all. Making smart and safe choices about activities is also key to preventing bleeds.
CAN FACTOR INFUSIONS BE DONE AT HOME?
While factor infusions may be given at your HTC or doctor’s office, many patients and their families choose to infuse factor treatment on their own. This allows people to treat most joint and muscle bleeds, as well as mouth and nose bleeds, at home. Remember that serious bleeds – in the vital organs – require immediate medical attention. Ask your HTC team for the signs of serious bleeds that you need to watch out for. Monitor every serious bleed, and keep your HTC team informed, so that your treatment plan can be optimized. At-home infusions require proper training, so speak to your HTC nurse to learn more.
FIRST AID TO HELP MANAGE BLEEDS: RICE
In addition to factor treatment, knowing the basics of first aid is important to managing bleeds. First aid can help slow bleeding for minor bleeds into joints or muscles. A good way to remember how to give first aid is the abbreviation RICE, which stands for Rest, Ice, Compression, Elevation. Here are the basics:
➥ Rest – When a bleed happens, that area of the body should be rested. For instance, someone with an ankle or knee bleed should limit activities. It may be useful for people with hemophilia to keep a set of crutches at home. A temporary half-cast or splint can also be used to limit movement, which may help limit a child from overusing an injured limb.
➥ Ice – Applying ice helps control swelling and reduce pain. Crushed ice in a plastic bag or a bag of frozen vegetables, wrapped in a towel, works well. Be careful not to apply the ice for too long as this can cause muscle weakness. Ten to 15 minutes, every two hours, is sufficient.
➥ Compression – Apply pressure on the bleed area to help "pinch off" the blood vessels and slow down the bleeding. Using an elastic bandage (tensor), wrap the injured part in a figure-eight pattern. Watch carefully for coolness, numbness, or a change in color in fingers or toes—if these occur, remove the bandage and re-wrap it less tightly. An alternative is a Tubigrip® sleeve. If the injury is very sore, compression may increase the pain; if so, rewrap the injury less tightly or remove the bandage altogether.
➥ Elevation – Elevating the area of a bleed (to a position higher than the heart) helps decrease the pressure in the blood vessels and slow the bleeding. Try using cushions or pillows to make this more comfortable.
If you have any questions on how to perform RICE or when it’s appropriate to do so, ask your HTC team.
OTHER TREATMENT OPTIONS
Factor infusions are the most common treatment for hemophilia, but not the only treatment available. There are also other medications that may be used for some patients.
Desmopressin is a synthetic drug based on a natural hormone called vasopressin. Desmopressin may be the treatment of choice for people with mild or moderate hemophilia A because it avoids the expense and potential risks of using clotting factor infusions. It is also particularly useful in the treatment or prevention of bleeding in carriers of hemophilia. It is not used for hemophilia B. Each patient’s response to desmopressin can vary significantly, so your or your child’s response needs to be tested before treatment begins.
Tranexamic acid and aminocaproic acid are two medications that work by helping to promote the stability of a blood clot. In hemophilia, each of these medications is usually used in specific short-term situations (e.g., oral bleeding during dental surgery, nose bleeds, menstrual bleeding) in combination with regular hemophilia treatment.
HOW TO IDENTIFY A JOINT BLEED: QUICK TIPS
EARLY SIGNS
➥ A tingling, bubbling sensation (but no real pain)
➥ Tightness and pain (but no visible signs)
LATER SIGNS
➥ Swelling at the joint and a hot feeling when the skin is touched
➥ Pain when bending or extending the joint
➥ Worsening swelling, and difficulty moving
REMEMBER: The earlier you treat a joint bleed, the better your chances of preventing serious damage.
There are two kinds of pain that a person with hemophilia may experience:
➥ Acute pain is short-term. It’s caused by bleeding into a joint or muscle and is usually the earliest sign of a bleed. A bleed that is not treated quickly can make the pain much worse. Even if there are no other obvious signs of bleeding, such as swelling, clotting factor therapy is recommended.
➥ Chronic pain is longer-term. It’s caused by long-term, or repeated, joint damage and typically affects older people with hemophilia who have ‘built’ up joint damage over the years.
The most effective way to manage pain in hemophilia is to prevent bleeds. This can help prevent repeated joint damage, which is a common source of chronic pain. And when a bleed does happen, it’s important to treat it early to help manage acute pain.
TREATING ACUTE PAIN
Pain from a bleed can be managed by giving factor replacement infusions to stop the bleeding. There are also non-medical techniques that can be used. Applying ice may also reduce acute pain. Supporting the arm or leg on a pillow, or in a splint, may also help. A relaxing activity or a warm bath can help soothe muscles, and take someone’s mind off their pain.
If your or a loved one is receiving regular factor infusion treatment and it does not seem to relieve the pain, contact your HTC immediately. It’s possible that inhibitors have developed that are interfering with treatment, or there may be another reason for the pain that’s not related to bleeding.
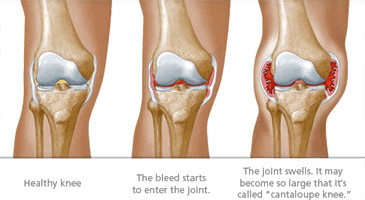
Why is joint disease a common complication in adults with hemophilia? Because there are many blood vessels in the synovium, or the lining of joints. The synovium is easily torn, which results in a bleed into the joint. When a lot of blood accumulates inside a joint, the synovium absorbs it. Iron from the blood builds up in the synovium, which thickens it and causes more blood vessels to form. This “thickening” is called synovitis, or joint swelling. One bleed makes another episode of bleeding more likely – starting a vicious cycle of joint damage.
Joint disease is much like arthritis: the joint, soft tissue, tendons and ligaments are damaged, and the damage gets worse over time. The result is pain, decreased range of motion, limited mobility and muscle atrophy (weakening). Because joint damage is progressive – the symptoms get worse as a person with hemophilia ages.
Some joints are more likely to be affected by bleeds than others, such as the knees, ankles and elbows because they are hinge joints and have little protection from side-to-side stresses. Ball-and-socket joints like the shoulder and the hip are well protected by large muscles, so bleed less often.
Joint disease, and the chronic pain that comes with it, can seriously impact a person’s quality of life. People may feel as though they can’t enjoy the same activities they used to, like riding a bike, going for a walk or doing everyday chores. Some people with more severe damage may need assistive devices. It’s important to talk to your doctor and HTC team about ways you can help prevent joint damage.
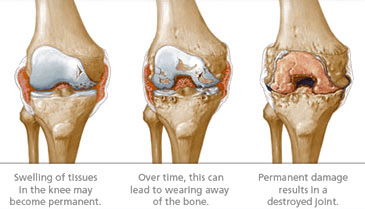
The most effective way to prevent joint damage is to treat bleeds immediately with clotting factor to stop the bleeding. Proper rest is also necessary, and follow up infusions may be needed, to help ensure that the joint properly heals.
It’s also possible to try to prevent bleeds from happening in the first place with regular prophylaxis therapy. People with moderate or severe hemophilia may receive factor concentrate, if they are a candidate for therapy, before they participate in sports or other activities which may place stress on joints and increase the risk of bleeds.
There are helpful tools available that can show you the impact nonadherence to a prophylaxis regimen can have on your joints. Talk to your doctor for more information about these tools.
OTHER WAYS TO MANAGE JOINT DISEASE
In addition to treating bleeds, physiotherapy can be beneficial to keeping joints and muscles protected. Physiotherapy can help to strengthen muscles around the joints so they bleed less frequently, as well as help prevent further injury. Because each patient’s situation is unique, a licensed physiotherapist who has experience treating people with hemophilia should prescribe specific exercises based on a detailed assessment of the patient’s condition. If you don’t already have one, your doctor or HTC can help you find a suitable therapist.
In some cases, joint disease progresses so far that it becomes painful or difficult to walk or do other daily activities. When this happens, it may be necessary to undergo one or more kinds of joint surgery, including:
➥ Joint replacement, or the surgical removal of a damaged joint and insertion of a new, artificial joint.
➥ Joint fusion, which uses special surgical tools to help mend the damaged section of a joint. This procedure fuses, or attaches, two bones on each end of a joint, eliminating the joint itself. Joint fusion helps a joint to regain its stability, bear weight better, and lessen pain.
Both procedures are performed by an orthopedic surgeon who works closely with a hematologist to manage bleeding during and after surgery. After surgery, physiotherapy is needed to help a patient strengthen the surrounding muscles and regain motion in the joint.
There may be other options your doctor recommends to help manage joint pain.
1. A tingling, bubbling sensation (but no real pain)
2. Tightness and pain (but no visible signs)
1. Swelling at the joint and a hot feeling when the skin is touched
2. Pain when bending or extending the joint
3. Worsening swelling, and difficulty moving
The earlier you treat a joint bleed, the better your chances of preventing serious damage.

A comprehensive care team is a group of health professionals who work in a Hemophilia Treatment Centre (HTC). Together, they collaborate to care for a patient and provide support for his or her family. Comprehensive care teams are also available to support carriers and their families. Each member of the team offers a different type of support: some help with medical issues, while others help with the emotional and social challenges that patients and their families often face. These issues evolve as a child gets older – from daycare to the teen years to adulthood – so the care provided by your team will also adapt to meet these changing needs.

1. Hematologist - a doctor who specializes in blood disorders, and who manages and directs the patient’s medical care.
2. Nurse coordinator, who is often most involved with hands-on treatment and education
3. Physiotherapist to help with joint and muscle problems that may develop
4. Social worker to help families deal with emotional, social and/or practical concerns

This team also works closely with:
1. Coagulation laboratory, a lab that does specialized blood clotting tests
2. Hematology laboratory (for all other blood tests)
3. Blood bank (for product storage)
4. X-ray department, for assessing joint condition
5. Dentist, especially one familiar with hemophilia

Depending on the patient’s needs, the team may also include:
1. Additional hematologists
2. Pediatrician (for younger patients)
3. Orthopedic surgeon
4. Gynecologist/obstetrician
5. Rheumatologist
6. Genetic counselor/geneticist
7. Psychologist
8. Hepatologist (liver specialist)
9. Ear/nose/throat specialist
THE MANY BENEFITS OF PHYSICAL ACTIVITY
The benefits of exercise to people with hemophilia are much the same as for those without the condition. It helps people maintain a healthy weight, promotes endurance, and helps keeps muscles strong. The added benefits in hemophilia are that a strong body helps protect it from bleeds – which is why regular exercise is a vital part of managing the condition.
THE BENEFITS OF EXERCISE: BODY, MIND, AND SPIRIT
Physical
Strong and flexible muscles support the joints, which helps prevent bleeds and joint damage.
Overall fitness Feeling fit and having energy helps reduce fatigue.
Maintaining a healthy weight Being at a healthy weight reduces the stress placed on the joints, which is especially important as a person ages.
Improved balance and coordination helps joints and muscles work better together, which in turn, help protect them from bleeds.
Psychological and social
Improved well-being
Sweating it out is a great outlet to help relieve stress, and relax the mind.
Self-esteem, confidence and FUN!
It’s fun to be active – for kids and adults! Playing sports, or doing any regular exercise, can boost self-esteem, promote social acceptance and provide a peer group to bond with.

CHOOSING THE RIGHT ACTIVITIES
While exercise and sports have many benefits for people with hemophilia, it’s important to choose activities wisely. Some high-impact activities are still considered too risky because of the higher risk of serious bleeding. Be sure to talk to your doctor and care team about what activities are best for you or your loved one. A physiotherapist experienced in working with hemophilia can also help develop an appropriate exercise program.
The World Federation of Hemophilia has put together a list of the top activities recommended by doctors who care for hemophilia patients, and the ones to avoid. You may find it to be a useful guide in choosing activities. Always talk to your doctor before starting a new activity or sport.
Swimming, Table Tennis, Walking, Fishing, Dancing, Badminton, Sailing, Golf, Bowling, Cycling
Boxing, Rugby football, Football, Karate, Wrestling, Motorcycling, Judo, Hang-gliding, Hockey, Skateboarding
What benefits are you seeking? Are they strictly physical, or social? Is your child competitive? How can you meet your child’s goals in a safe manner?
When should infusions be given around activity? If your child is on prophylaxis therapy, talk to your HTC team about when to schedule infusions (e.g., before a sports practice).
Is it an activity you can do as a family? Doing activities together can help parents more closely supervise and monitor their child.
Does your child have well-developed reflexes and co-ordination? If your child is young and still developing these skills, they are at a greater risk for a fall or injury. Talk to your HTC physiotherapist about activities that may be more suitable, and exercises that can help improve reflexes.
Does your child have a ‘target’ joint? A target joint is one that has suffered repeated bleeds. Ensure it is safely protected during activities (e.g., with a brace or appropriate footwear).
What is the speed and potential body contact involved in the activity? The higher the speed, and potential for contact (e.g., football, rugby, hockey), the greater the risk for injury and bleeds. Have a frank talk with your child about the potential risks, and whether they can find enjoyment in another, safer sport.
Are there sports to avoid for a target elbow, ankle or knee joint? Racquet sports with lots of start-and-stop motion can place these joints at a higher risk of bleeds, so should be avoided.
"Adapted from All About Hemophilia: A Guide for Families, Chapter 12: Physical Activity, Exercise and Sports."
As people with hemophilia age, their risk for joint damage increases. As a result, they may experience chronic pain and have reduced mobility and range of motion. Yet, it’s still important to remain active to help strengthen joints and muscles, maintain a healthy weight, and provide an outlet for any stress or tension.
Choose activities that ‘go easy’ on the joints. Since knees, elbow and ankles are often affected by joint damage, activities like jogging, basketball, or soccer are not ideal. Instead, consider these:
➥ Walking
➥ Swimming
➥ Yoga or pilates
➥ Cycling
➥ Strength (weight-bearing) exercise. If you’re unsure how to get started, ask a friend or someone at your local gym.
➥ If you want to change it up – throw in a dance class or a game of bowling!
For you or your child, exercise is all about choosing wisely, taking precautions, and having FUN! Your doctor or physiotherapist can help you select the right activities, and help adjust the infusion schedule, if needed.